Glen Cousquer BSc (Hons) BVM&S CertZooMed MRCVS
Introduction
A six year old male spur thighed tortoise (Testudo graeca graeca) was presented in mid February with rat bite injuries to its limbs, tail and shell. Such injuries are common in hibernated tortoises, where no precautions are taken to keep the tortoise safe from predation. This case report describes the presentation and treatment of the tortoises injuries.
Presentation
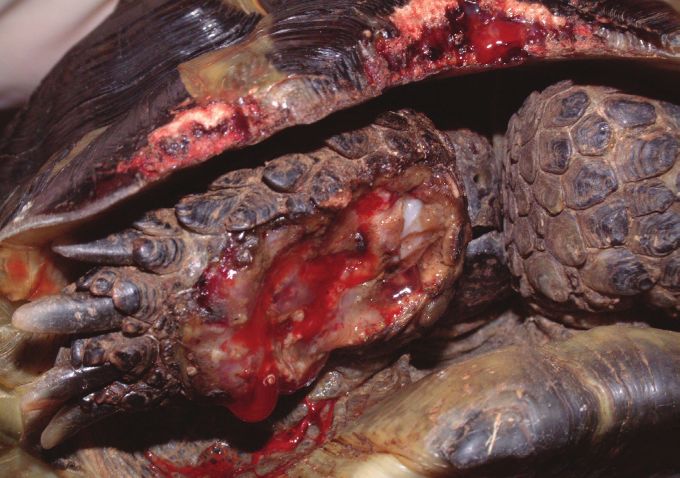
The tortoise presented in mid February, having recently emerged from hibernation. On presentation the tortoise weighed 510g and was found to have a deep and extensive soft tissue wound to the anterior aspect of the right foreleg (Figs 1-2). The wound stretched from above the elbow to the level of the carpus and extended down into the elbow joint, as indicated by the presence of synovial fluid within the wound. The wound was contaminated with soil and showed extensive tissue necrosis. Gnaw wounds to the cranial rim of the carapace were noted (Figs 1-2). A second extensive wound running the length of the tail, from the tip up onto the caudal aspect of the left thigh was also noted, together with a smaller wound to the caudal aspect of the right thigh (Fig. 3).
Initial first aid treatment consisted of wound lavage with dilute povidone iodine. Silver Sulfadiazine cream (Flammazine; Solvay-Duphar) was applied to all wounds and a hydrocolloid dressing (Comfeel, Coloplast) applied to the right foreleg. Antibiotic treatment was initiated with Marbofoxacin (5mg/kg /m), analgesia with Meloxicam (0.2 mg/kg s/c).
The following day (day 2), the tortoise was anaesthetised in order to perform a more thorough wound debridement. General anaesthesia was induced with Propofol (10mg/kg), by intravenous injection; the tortoise was intubated and anaesthesia maintained with Isofurane (1-3%). An oesophageal feeding tube was placed to facilitate supportive feeding, fluid and drug administration. The wounds were again flushed and debrided. The tail wound was dressed with a cut section of hydrocolloid dressing (Comfeel, Coloplast) that was sutured in place over the wound (Figs 4-8). The wound to the right thigh was similarly cleaned and debrided. The cavity was then packed with silver sulfadiazine cream.
Careful assessment of the injuries to the right forelimb confirmed the severity and extensiveness of the tissue necrosis. The owners were advised that the chances of saving the limb were poor and that the speediest recovery could be obtained by opting for limb amputation.
Broad spectrum antibiotic cover was continued with Marbofoxacin (5 mg/kg i/m sid). Pain relief was also continued with Meloxicam (0.2 mg/kg s/c sid).
The wound to the right forelimb was re-examined on day 5 and was found to have deteriorated (Fig. 9). Consent for the amputation was obtained. The tortoise was re-anaesthetised on day 5 and the limb prepared for surgery (Fig. 10). A high amputation was performed through the proximal third of the humerus. The muscle bodies were sutured over the remaining length of humerus and the skin closed with horizontal mattress sutures (Fig. 11). The surgical wound was protected with a coat of pulverised aluminium (Aluspray; Vétoquinol) (Fig. 12).
Antibiotic cover with Marbofoxacin was continued, in combination with Cephalexin (30mg/kg i/m sid).
The tortoise failed to eat voluntarily or produce faeces until day 8. During this time support feeding was provided via the oesophagostomy tube, using a mixture of a high fibre herbivore recovery diet (Critical Care; Oxbow) and an electrolyte and probiotic solution (Avipro; VetArk). A faecal examination on day 8 revealed no gut parasites.
The tortoise was returned to the owners for home care on day 9. Antibiotic and anti-inflammatory cover were continued for a further ten days.
The tortoise re-presented on day 15 for a post-operative examination and wound re-dressing. The tortoise was again anaesthetised. The surgical wound to the right foreleg was healing well. The tail dressing was removed, revealing a healthy bed of granulation tissue (Fig. 13). The tail was re-dressed as before (Fig. 14). The wound to the right thigh appeared healthy and was cleaned and packed with silver sulfadiazine cream. The oesophageal feeding tube was removed as the tortoise was now eating and drinking well. An improvised limb prosthesis was applied to the anterior plastron in the midline to help raise the tortoises shell off the ground, thus facilitating locomotion. For this purpose the bowl of a plastic spoon was glued to the plastron with methylmethacrylate (Fig. 15).
The tortoise was seen again on day 30. The dressing over the tail was removed. Both the tail wound and the wound to the right thigh were healing well. The limb prosthesis was removed and replaced with a smaller piece of resin. The spoon raised the shell too far off the floor and did nothing to facilitate locomotion.
The tortoise was re-examined later in the year, on day 92. All wounds had healed and the tortoise was doing very well (Fig. 16).
Discussion
Rat bites are most commonly reported in reptiles that are fed rats as prey (Barten, 2006b; Schilliger, 2004b). Tortoises are, however, also vulnerable to rat attacks, particularly during the winter months when many tortoises undergo hibernation. Rat bite trauma is, unfortunately, a common presentation in post-hibernation animals (McArthur et al., 2004). The exposed surfaces of the fore and hind limbs, as well as the tail, are most commonly affected, although eye and head injuries are also occasionally seen (McArthur et al., 2004). Gnaw injuries to the shell may also be seen, as in this case.
On presentation, these patients will require a thorough examination and assessment to establish the status of the patient and the extent of their injuries. Initial treatment will aim to stabilise the patient and will consist of fluid therapy, analgesia, rewarming and temporary wound care.
Warming and fluid therapy is recommended in most patients, and indeed necessary to reverse hibernation in patients that have only just emerged from hibernation (McArthur et al., 2004). Patients should be maintained within their preferred optimal temperature range, which, in Testudo species, is usually between 20-32°C. Core body temperature can be monitored using a digital cloacal temperature measuring probe and should be as close as possible to the preferred body temperature (around 26°C for Testudo species).
Fluid therapy can be administered either orally or by epicoelomic injection. The provision of warm baths will allow fluid uptake via both the oral and cloacal routes, as well as encouraging the tortoise to void faeces and urine. In the post hibernation tortoise, the placement of an oesophagostomy tube will allow the provision of both fluid and nutritional support. This can prove particularly useful in tortoises showing post hibernation anorexia. A high fibre diet, suitable for convalescing herbivores, such as rabbits, and mixed with a suitable rehydration formula, can be administered via the oesophagostomy tube. Care should be taken to keep the tube clean and free from blockages. After each feeding the tube should be flushed with water and the tube plugged.
The provision of antibiotics may need to be delayed until samples have been taken for culture and sensitivity. This step should not be overlooked, and is indeed strongly recommended, as chronic wounds can be infected with a range of bacteria, of uncertain antibiotic sensitivity. The possibility of mycotic and / or mycobacterial infection should also be considered. Cytological sample collection may be used to guide initial antibiotic therapy (Mitchell et al., 2004). Initial treatment can be instituted with a cephalosporin antibiotic such as Ceftazidime (20mg / kg every 78hrs), which is widely distributed throughout the body (McArthur et al., 2004), or Cephalexin (30mg / kg twice daily). The cephalosporin antibiotics show activity against anaerobes as well as aerobes and this represents a distinct advantage over aminoglycoside and fuoroquinolone antibiotics (McArthur et al., 2004). Combination therapy using a third generation cephalosporin together with a fuoroquinolone or an aminoglycoside is reported to be synergistic (Mayer & Nagy, 1999). Enrofoxacin can be used at 10mg / kg once daily (Raphael et al., 1994) or Marbofoxacin at 5-10mg / kg once daily. In this case drug availability influenced the selection of antibiotic therapy. Topical therapy using medications such as silver sulfadiazine, dilute chlorhexidine and acrifavine ointment are also proposed (Fraser & Girling, 2004).
Where further evaluation and characterisation of a contaminated wound is indicated, the combination of a cytologic exam, microbiologic culture, and biopsy for histopathology is recommended (Mitchell et al., 2004). Such further tests are indicated in all wounds demonstrating delayed wound healing, as well as those where neoplasia or nutritional deficiencies are suspected.
Analgesia should be provided to counter the pain associated with extensive soft tissue and orthopaedic injuries. McArthur et al. (2004) recommends the use of the non steroidal anti-inflammatory drug, Carprofen, as a single subcutaneous injection at 2-4mg / kg. Concerns over the possibility of reduced renal perfusion in these patients may justify restricting pain relief to a single injection (McArthur et al., 2004). Opioid partial agonists such as Butorphanol and Buprenorphine can also be used (McArthur et al., 2004). In this case pain relief was provided with Meloxicam at 0.2 mg / kg once daily. This was continued for a total of 19 days without any obvious side effects.
Wound management should be pursued aggressively. All prey bite injuries should be managed as contaminated wounds (Mitchell et al.., 2004). Wounds less than 6-8 hours old may, however, be suitable for primary closure; in which case care should be taken to evert the skin edges (Mitchell et al., 2004). Older wounds must be assessed carefully. In the first instance, the wounds should be thoroughly flushed and vigorously debrided. This is particularly important as rat bites are potential sources of mycobacteriosis, to which chelonians are known to be susceptible (McArthur et al., 2004). Wound flushing and debridement should be performed under general anaesthesia. Sedation can be induced using a midazolam and ketamine combination, and anaesthesia achieved by intubating and ventilating with a volatile agent such as Isofurane or Sevofurane (McArthur et al., 2004). Alternatively, anaesthesia can be induced using Propofol at 10-14mg / kg, as described here.
Surgical debridement of all necrotic and non viable tissue should be performed at the earliest opportunity and repeated until healthy tissue margins are established. Severely affected limbs should be immobilised. This can be achieved by flexing the limb, folding it back into the shell and taping across the opening between the plastron and carapace. Extensive injuries to the limbs may warrant surgical amputation in order to produce a healthy surgical wound, as occurred in this case.
Open wounds should be protected against dessication and secondary infection. Such wounds may be protected with a gel suited to open wound management and covered with a moisture vapour permeable dressing. Alternatively, they can be dressed with a hydrocolloid dressing that can be secured over the wound with simple interrupted sutures. Such dressings ensure that the wound is kept clean and moist, creating an optimal environment for wound healing. These dressings appear to be well tolerated and resistant to the daily wetting that occurs when the tortoise is bathed. It is important that baths are kept short (approximately 5 minutes) in order to minimise exposure to water and any excreta produced by the tortoise. Where additional debridement is required, some authors propose the use of wet to dry bandages consisting of surgical gauze soaked in physiological saline or a 1:40 solution of warmed chlorhexidine (Mitchell et al., 2004). The frequency of dressing changes will be dictated by the extent of any wound discharge. Granulating wounds producing minimal wound discharge can be changed every 4-7 days.
Wound healing in tortoises
In chelonians, the skin structure has evolved to resist the aggressive challenges of a range of hostile environments. Their natural environment is typically hot, arid and abrasive and the tortoises skin therefore needs to be resistant to mechanical trauma, heat and intense ultraviolet radiation. The skin that covers the tail, head, neck and limbs is, in places, heavily keratinised and protected by scales of ectodermal origin (Cooper, 1992; Davies,1981). The reptilian epidermis is composed of three main layers; the beta-keratin layer is the most superficial layer and overlies the mesos layer and the alpha- keratin layer (Fraser & Girling, 2004). The alpha-keratin layer is supported by the underlying stratum germinativum. The epithelium that overlies the chelonian shell is generally thickest and contains layers of keratin overlying a pseudostratified layer (Fraser & Girling, 2004). The deeper dermis is derived from embryonic mesoderm and provides, support, nourishment and colour to the epidermis (Davies, 1981). The dermis contains connective tissue, vascular tissues, sensory structures and dermal bone (osteoderms). Osteoderms are composed of a mixture of spongy and compact bone and, in tortoises, have fused with the ribcage and spine, expanding to form the plates of bone that make up the chelonian carapace and plastron (Fraser and Girling, 2004).
Wound healing in tortoises proceeds by a process of granulation, epithelialisation and wound contraction. The process of wound healing in reptiles is further described by Bennet & Mader (1996) and Mitchell et al. (2004). Skin wounds generally take several weeks to heal and the process has been shown to be temperature dependent (Smith et al., 1988; Cooper, 1992).
Prevention of rat bite injuries
The choice of hibernacula should take into account the possibility of rat incursion. Insulated boxes have, historically, been popular with UK tortoise keepers but leave the potential for rat trauma. Many authors now prefer to use refrigerators as a hibernation enclosure. These are eminently suitable for the purpose of hibernating a number of tortoises, providing air is changed on a daily basis and the temperature closely monitored. Whatever the method of hibernation, the container and building should be made rat proof. Regular checks should be made, particularly where insulated boxes are placed in lofts or garages. In addition to visual checks, tortoises should be weighed during their hibernation and the ambient temperature carefully monitored to ensure that it remains within the range 2-9°C. Weight loss during hibernation should not exceed 8-10% body weight.
Conclusion
Rat bite injuries are commonly sustained by hibernating tortoises. Such injuries are therefore commonly seen in post-hibernation tortoises. Soft tissue injuries are typically sustained to the tail, fore and hind limbs, although the head and neck may also be involved. Our understanding of wound healing in reptiles is still in its infancy and, to date, many of the therapeutic methods used in reptiles have been adopted from human, mammalian or avian species. Aggressive wound management techniques are indicated and can often involve limb amputation. Even very extensive soft tissue wounds can respond well to treatment.
References
Barten, S.L. (2006a). Shell damage. In: Reptile Medicine and Surgery. Ed: D.R. Mader Elsevier, St Louis, Missouri, USA, pp. 893-899.
Barten, S.L. (2006b). Bites from prey. In: Reptile Medicine and Surgery. Ed: D.R. Mader Elsevier, St Louis, Missouri, USA, pp. 747-750.
Bennett, R.A. & Mader, D.R. (1996). Soft tissue surgery. In: Reptile Medicine and Surgery. Ed: D.R. Mader. W.B. Saunders, Philadelphia, USA, pp. 287-298.
Cooper, J.E. (1992). Integument. In: BSAVA Manual of Reptiles. Eds: P.H. Beynon M.P.C. Lawton & J.E. Cooper. BSAVA, Cheltenham, UK, pp. 73-79.
Davies, P.M.C. (1981). Anatomy and Physiology. In: Diseases of the Reptilia. Eds: J.E Cooper & O.F. Jackson. Academic Press, London, UK.
Fraser, M.A. & Girling, S.J. (2004). Dermatology. In: BSAVA Manual of Reptiles Second Edition. Eds: S.J. Girling & P. Raiti. BSAVA, Gloucester, UK, pp. 184-198.
McArthur, S. & Hernandez-Divers, S. (2004). Surgery. In: Medicine and Surgery of Tortoises and Turtles. Blackwell Publishing, Oxford, UK, pp. 403-464.
Mayer, I. & Nagy, E. (1999). Investigation of the synergistic effects of aminoglycoside-fuoroquinolone and third generation cephalosporin combinations against clinical isolates of Pseudomonas spp. J. Antimicrob. Chemother. 43(5): 651-657.
Mitchell, M.A. & Diaz-Figueroa, O. (2004). Wound management in reptiles. Vet. Clin. North Am. Exot. Anim. Pract. 7(1): 123-140.
Raphael, B., Papich, M. & Cook, R.A. (1994) Pharmacokinetics of enrofoxacin after a single intramuscular injection of enrofoxacin in Indian Star Tortoises. Journal of Zoo and Wildlife Medicine 25: 88-94.
Schilliger L. (2004). Fractures de la Carapace. In: Guide Pratique des Maladies des Reptiles en Captivité. Editions Med’Com, Paris, pp. 78-80.
Schilliger L. (2004b). Morsures. In: Guide Pratique des Maladies des Reptiles en Captivité. Editions Med’Com, Paris, pp. 122-123.
Smith, D.A., Barker, I.K. & Allen, O.B. (1988). The effect of ambient temperature and type of wound on healing of cutaneous wounds in the common garter snake (Thamnophis sirtalis). Canadian Journal of Veterinary Research 52: 120.
Acknowledgement
Reprinted from Cousquer, G. Post-hibernation management of rat bite injuries in a spur-thighed tortoise (Testudo graeca). World Wide Wounds, February 2007, with permission from the Publishers. Available from:
www.worldwidewounds.com/2007/february/Cousquer/Tortoise-Rat-Bite-Injuries.html
Testudo Volume Six Number Five 2008
Top